Urethroplasty is an open surgical reconstruction or replacement of the urethra that has been narrowed by scar tissue and spongiofibrosis (urethral stricture). Urethroplasty is the gold standard for urethral reconstruction with the best and most durable results.
For patients who have failed prior urethroplasty, or where the urethra and local skin are severely scarred, a staged urethroplasty is usually indicated.
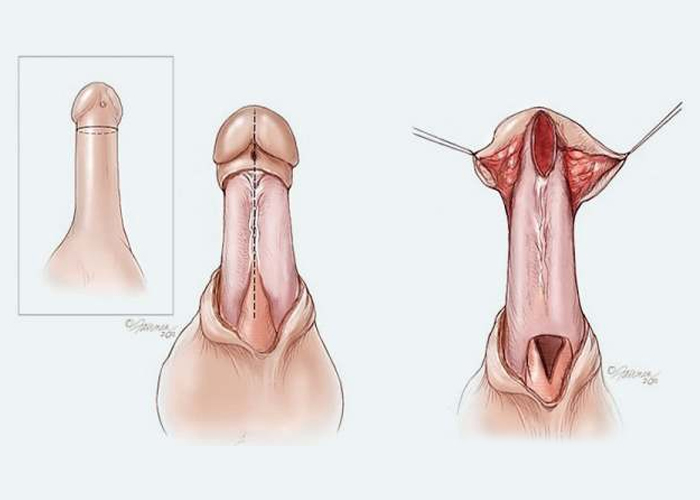
Here, the scarred urethra is typically surgically excised, and in its place, a buccal or skin graft is placed. This replaced urethra is left open to the air to heal over the next few months. The meatus (pee hole) is often placed in front or under the scrotum causing patients to sit to urinate for a few months. Once the graft is soft and well healed, the patient undergoes a second ("staged") surgery to roll the graft up into a tube to reconstruct the urethra. A staged urethroplasty can require more than two steps and more than one phase of grafting. Staged urethroplasty is typically reserved for the worst urethral strictures.
A 'ureteral stent' or 'ureteric stent' is a thin, hollow tube inserted into the ureter. Ureters are thin tube-like-organs which connect kidneys to the urinary bladder, to allow urine flow from the kidney. The stent is longer than the actual ureter and tube-ends are usually coiled. These coiled ends stay in the kidney on one side, and bladder on the other side, so as to minimise chances of its displacement. The length of the stents used in an adult patients varies between 24 to 30 cm. Stents come in differing diameters or gauges, to fit different sized ureters. Stents also contain small openings in their walls towards the ends, known as ‘fenestrations’. These fenestrations aid in the passage of urine.